Great article I thought I’d share by Brad Flansbaum
IF CONGRESS PLANS ON FIXING THE RACS IN 2015, THEY NEED TO READ THIS FIRST!
• February 24, 2015
The recent increase in observation stays has led to a surge in federal oversight and scrutiny. We have covered the dispute on the blog before. And yes, as the facilitators of the process, the recovery audit contractors (RACs) continue to receive the lion’s share of critical attention—especially with congress.
In our attempts to resolve the issue of appropriate in versus outpatient hospital stay designations, pressed inpatient facilities endure overwhelmed administrative law judges (ALJ) and employ hospital FTE resources they cannot spare.
The RACs get the spotlight for what they do, or if you need reminding, don’t. Moreover, we can only speculate on the veracity of the data and how their auditors perform. Previously, we possessed only aggregated, somewhat filtered information released by the government. Until now.
The Journal of Hospital Medicine has released a first of a kind paper exploring the above.
Given the importance of RAC auditing pressure in the growth of hospital observation care, the study investigators conducted a retrospective descriptive study of all RAC activity for complex Medicare Part A alleged overpayment determinations at the Johns Hopkins Hospital, the University of Utah, and University of Wisconsin Hospital and Clinics for calendar years 2010 to 2013.
To set the frame:
[…} there are increasing concerns that the RAC program has resulted in overaggressive denials. Unlike other Medicare contractors, RAC auditors are paid a contingency fee based on the percentage of hospital payment recouped for cases they audit and deny for improper payment. RACs are not subject to any financial penalty for cases they deny but are overturned in the discussion period or in the appeals process. This may create an incentive system that financially encourages RACs to assert improper payment, and the current system lacks both transparency and clear performance metrics for auditors.
What did the study show?
• RACs audited 8% of Medicare encounters (8,110/101, 862), a rate 25 times the overall manual audit rate of 0.3% cited by CMS
• RACs alleged overpayments in a third of those encounters
• While not reported in appeals data, hospitals won 33% of the alleged overpayment claims in thediscussionperiod, accounting for over 2/3 of decisions in favor of the hospitals.
• Counted as “inappropriate” and considered a recovery by the RACs, AMCs resubmitted 50% of settled, contested claims under Part B, instead of Part A Medicare (41% of total).
• No overpayment determination questioned the need for care, rather how the care should be classified.
• Each institution used 5 full-time staff for the audits
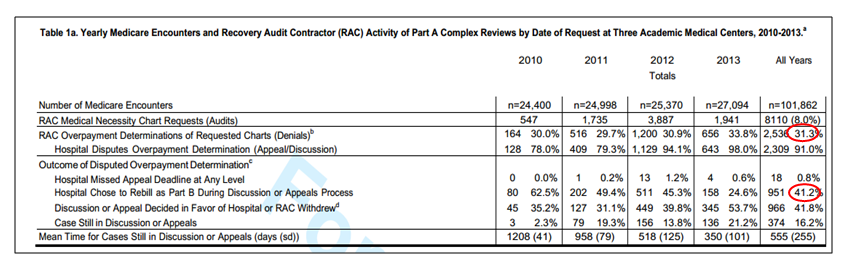
The 33% overturn rate found in the discussion period represents errors committed by the initial RAC auditors—a disturbingly high percentage. Most objective assessors of the process would not consider this discussion part of the appeals course. Ill-advisedly, these denominator cases do not appear in CMS or OIG reports of RAC activity.
Based on their methods, CMS “underestimated” the true overturned denial rates at the three study hospitals, and by proxy, other institutions undergoing the same reviews. Where I come from, we call that buffing the data. Getting CMS RAC reform measures to the fore will hinge on auditor accuracy. Unless CMS includes discussion period action in the scorecard, we will continue to assess the RAC enterprise with one eye open.
The study hospitals are also being denied timely due process and payments for services delivered. Hospitals currently face an appeals procedure that, on average, exceeds 500 days. Notably, Medicare is not adhering to its own dictates, which require appropriate agencies to hear appeals in a prompt manner.
I also encourage you to review the tables more in depth and note the audit quality at the three intuitions. They varied significantly, indicating either a lack of standards or a misapplication of the rules by the RACs.
Finally, hospitals, no doubt, would rather reallocate FTEs to other meaningful tasks. We need personnel on the front lines, not in the back rooms counting beans and dredging data.
I applaud the investigators for shedding light on the subject of RAC audits. The new information will assist in a system redesign with a focus on efficiency and sanity: one hinging on more transparency, timely review, sensible look back periods, and with a revised contingency fee schema.
BONUS: If you wish to read a succinct summary on potential RAC next steps, see this MedPAC 2015 deck.

