
Clinical Appeals Case Study
Challenge
The client is suffering under an “onslaught” of denials and while struggling to keep up, they also would like to understand the exact reason for the denials and their fiscal impact on the client.
Solution
Claim WRX application is deployed in 9 days after the facility required EHR training. The client creates an EHR work queue where staff can pass us work as they need help. Those cases are:
- Assessed for appeal strategy
- Appeal Written within 5 days or sooner
- Appeal Over Reading for Strategy, Accuracy, Grammar (Industry Outlier)
- Client Delivery of “Appeal Story/Report” and Appeal Letter
- Executive Reports Delivered Monthly (Online Meetings Available)
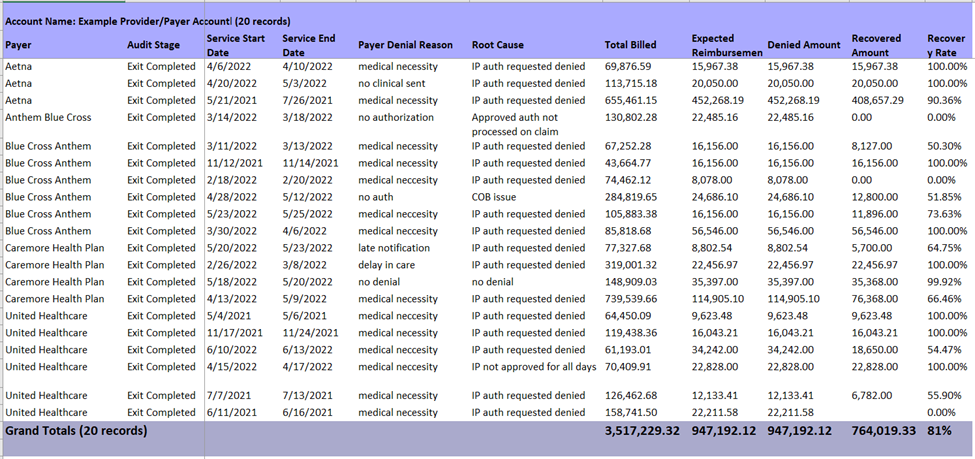
These break down for the client:
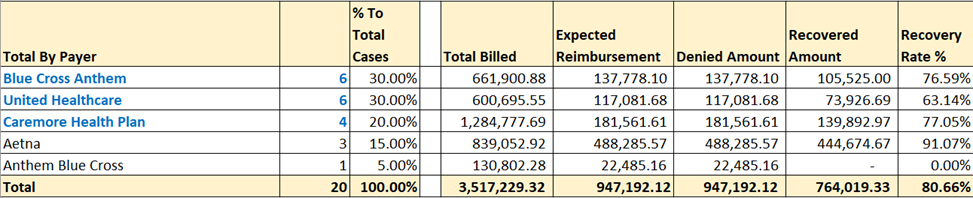
- Total # of cases for the previous month by payor with fiscal impact (pipeline report)
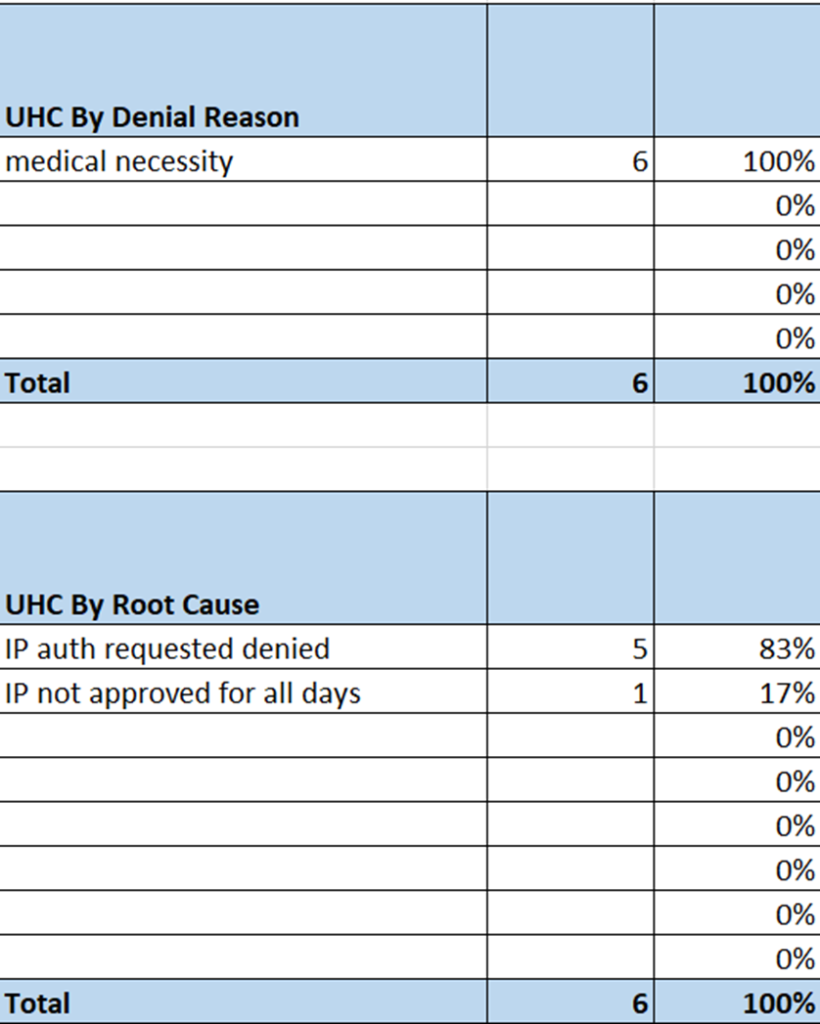
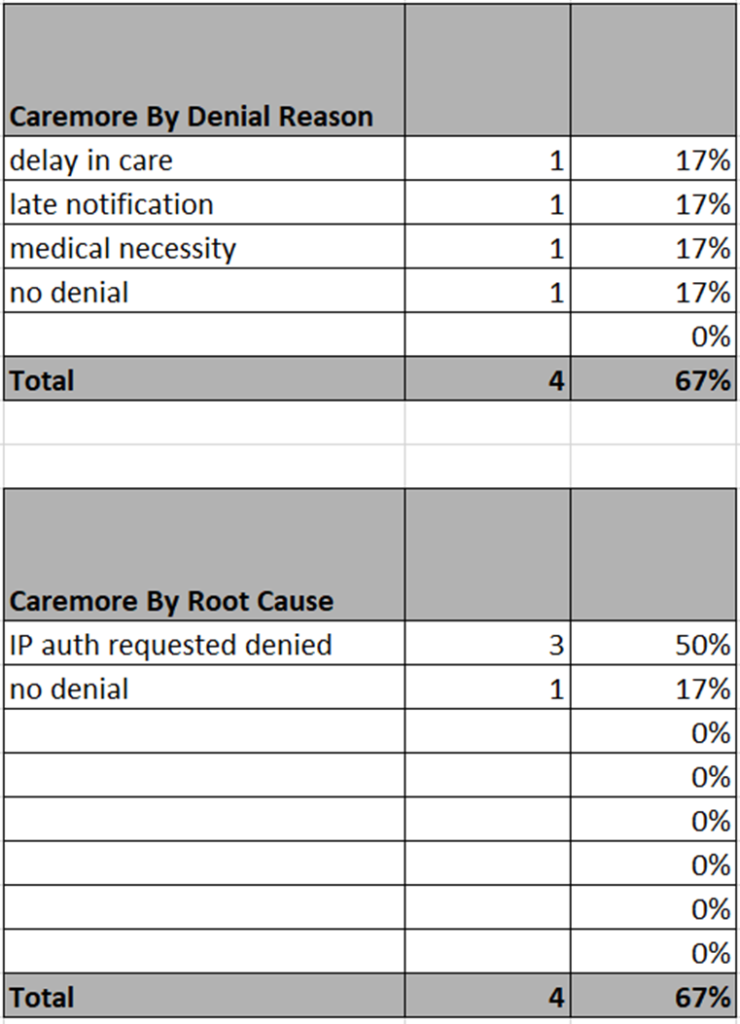
- Total # of cases by “Denial Reason” for the previous month by payor with the fiscal impact
- Total # of cases by “Root Cause” for the previous month by payor with the fiscal impact
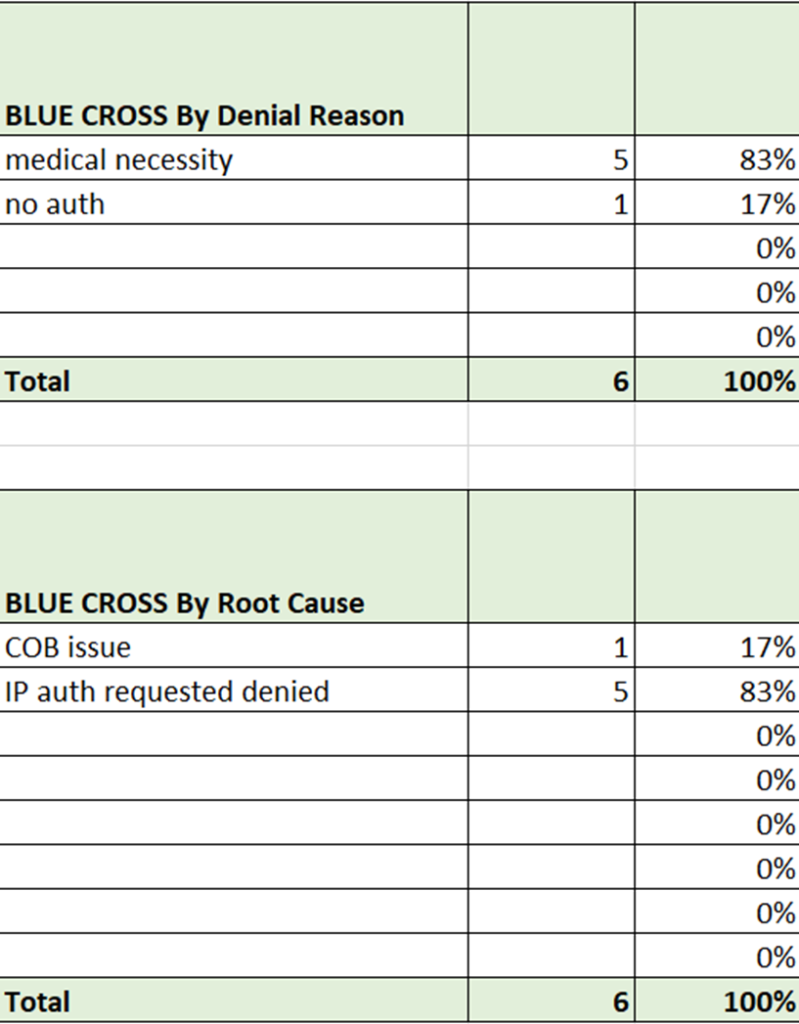
- Finally, a short series of the “Top 3 Payor Activity” for the previous month by payor with “Denial Reason vs. Root Cause”
- All reporting can be customized if needed
Results
- Total Cases Represented = 20
- Total Billed Amount $ 3,517.229.32
- Total Expected Reimbursement (after adjustments) = $947,192.12
- Total Recovered Amount after Appeal Exhaustion = $764,019.33 (80.66%)
- 70% of Denial Reasons are declared Medical Necessity
- 80% are “actually” IP auth requested denied as the “root cause”
- The Top 3 Payor Activity Reports show these stats broken down again by Payor
Client Impact
80.66% recovery ($764,019.33) of denied dollars using a variety of appeal techniques in conjunction with the creation of the “story” of why the denial actually occurred
Detailed feedback generated by Individual Case Reports and Executive Level Reporting delivered to clients (Online Meetings Available)
Stats

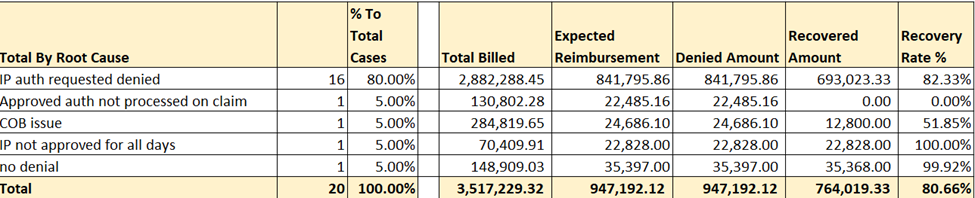
Top 3 Payor Activity (Denial Reason vs. Root Cause)
For over 20 years we have been helping payors and providers manage Payment Integrity, Care Quality, and Audits. We continue to innovate and are excited to announce our latest advanced technology platform, Claim WRX We custom tailor our solutions by integrating Claim WRX, with your team and augmenting our staff when needed. Together we help you successfully manage the rising onslaught of Denials and Audits facing healthcare. Built on the Salesforce Platform, we require no IT Integration, have Military Grade Security, and a proven record of success.

